
Advice for your Recovery Support Person – Spouse, Friend or Family members
If your loved one is preparing to undergo a plastic surgery procedure, you may be feeling a mix of emotions – excitement for the positive changes to come, but also apprehension about the recovery process. As a spouse, friend, or family member, your support during this time is invaluable. Your presence, encouragement, and practical assistance can make a world of difference in ensuring a smooth and successful recovery.
This guide created by Chester Consultant Plastic Surgeon Anca Breahna and her team is designed to help you understand your role as a recovery support person and provide you with the tools and knowledge you need to offer the best possible care. Whether your loved one is undergoing a breast enhancement, reduction, or uplift; a tummy tuck or mummy makeover; a menopause makeover; or blepharoplasty (eyelid surgery), this resource will give you procedure-specific advice and tips to help you during the recovery journey together.
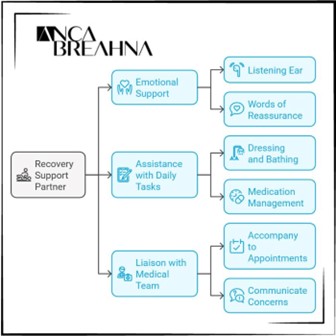
The Role of a Recovery Support Partner
As a recovery support partner, you play an important role in your loved one’s post-operative journey. Your involvement and dedication can significantly impact their physical and emotional well-being, helping them navigate the challenges of recovery with greater ease and comfort.
One of the most essential aspects of your role is providing emotional support and encouragement. Undergoing a surgical procedure can be a vulnerable and sometimes overwhelming experience, and your loved one may face moments of frustration, discomfort, or uncertainty. By offering a listening ear, a comforting presence, and words of reassurance, you can help alleviate their concerns and boost their confidence in the healing process.
In addition to emotional support, you’ll also be instrumental in assisting with daily tasks and post-operative care. This may include helping your loved one with dressing, bathing, and mobility, as well as ensuring they take their medications as prescribed and adhere to any specific care instructions provided by their surgeon. Your attentiveness and willingness to lend a helping hand can greatly contribute to their comfort and recovery.
Another key aspect of your role is serving as a liaison between your loved one and the medical team. You may be responsible for accompanying them to follow-up appointments, communicating any concerns or questions to the surgeon or nursing staff, and relaying important information back to your loved one. By staying informed and engaged, you can help ensure that any potential issues are addressed promptly and effectively.
Throughout the recovery process, it’s essential to remain patient, empathetic, and adaptable. Each person’s healing journey is unique, and there may be unexpected challenges or setbacks along the way. By maintaining a positive attitude, celebrating small victories, and adjusting your support to meet your loved one’s evolving needs, you can create a nurturing environment that promotes both physical and emotional healing.
What to Expect after Plastic Surgery
Recovering from plastic surgery is a gradual process that requires patience and proper care. As a support person, knowing what to expect during the first week after surgery can help you better assist your loved one throughout their recovery journey.
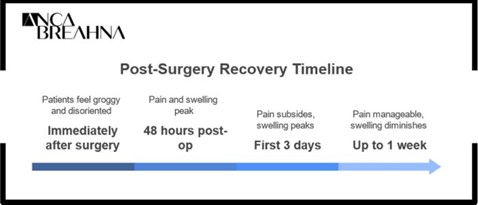
Here’s a general timeline of what patients may experience during the first 7 days post-op:
First 24 Hours:
- Immediately after surgery, patients may feel groggy, disoriented, or experience some nausea as a result of the anaesthesia.
- Pain, swelling, and discomfort are common and can be managed with prescribed pain medication.
- Patients should rest and sleep as much as possible, keeping their head elevated to minimise swelling.
- Dressings or compression garments may be in place to protect the surgical site(s) and promote healing.
48 Hours Post-Op:
- Pain and discomfort may peak during this time, but can still be controlled with medication.
- Swelling and bruising may become more noticeable, which is a normal part of the healing process.
- Patients should continue to rest and limit their physical activity, avoiding any strenuous tasks or movements.
- Gentle walking around the house is encouraged to promote circulation and prevent complications like blood clots.
First 3 Days:
- Pain and discomfort should start to subside gradually, although some soreness may persist.
- Swelling and bruising may continue to develop, often peaking around day 3 or 4.
- Patients may experience some itching or numbness around the surgical site(s), which is a sign of the healing process.
- Continued rest is essential, with short walks and light activities as tolerated.
- Patients should stay hydrated and maintain a healthy, balanced diet to support healing.
Up to 1 Week:
- Pain should be more manageable, and patients may begin to taper off pain medication as directed by their surgeon.
- Swelling and bruising should start to diminish, although some residual discolouration may persist for several weeks.
- Patients may feel more comfortable engaging in light activities, such as short walks or gentle stretches, as advised by their surgeon.
- Follow-up appointments with the surgeon will be scheduled to monitor progress and address any concerns.
- Compression garments or dressings may still be required to support the healing process and minimise swelling.
It’s essential to remember that every patient’s recovery experience is unique, and the timeline may vary depending on the type of procedure, individual healing factors, and adherence to post-operative care instructions. Some patients may feel better sooner, while others may require more time to recover.
As a support person, your role is to provide comfort, assistance, and encouragement throughout the first week and beyond. Help your loved one stay on top of their medication schedule, ensure they get plenty of rest, and assist with daily tasks as needed. Be patient and understanding, as the recovery process can be physically and emotionally challenging at times.
If you notice any signs of complications, such as excessive pain, swelling, redness, or discharge from the surgical site(s), contact Anca Breahna’s team immediately for guidance.
Responsibilities and Recommendations for the Support Person
Your responsibilities extend beyond providing emotional support and encouragement; you’ll also be instrumental in assisting with daily tasks, post-operative care, and ensuring your loved one follows their surgeon’s instructions. Here are some key responsibilities and recommendations to keep in mind:
- Assist with daily activities: In the early stages of recovery, your loved one may have limited mobility and energy. Help them with tasks such as dressing, bathing, and preparing meals. If they have children or pets, you may need to take on additional responsibilities to allow them ample time to rest and recover.
- Manage pain and discomfort: Ensure your loved one takes their prescribed pain medication on schedule and as directed by their surgeon. Help them find comfortable positions for rest and sleep, using extra pillows for support if needed. If they experience severe or unmanageable pain, contact Anca Breahna’s team for guidance.
- Encourage rest and relaxation: Create a peaceful and nurturing environment at home, minimising stress and distractions. Encourage your loved one to rest as much as possible, especially during the first 72 hours after surgery. Help them find enjoyable and relaxing activities that don’t require much physical exertion, such as listening to audiobooks, practicing gentle breathing exercises, or engaging in light conversation.
- Monitor swelling and bruising: Swelling and bruising are normal parts of the healing process, but it’s essential to keep an eye on their progression. If you notice any excessive swelling, redness, or discharge from the surgical site(s), inform the surgeon promptly. Assist your loved one with applying cold compresses or other recommended treatments to manage swelling and discomfort.
- Promote a healthy lifestyle: Support your loved one’s healing by preparing nutritious meals and encouraging them to stay hydrated. As they begin to feel better, help them incorporate light exercise and gentle movements into their routine, as advised by their surgeon. This can help improve circulation, reduce the risk of complications, and support the healing process.
- Attend follow-up appointments: Accompany your loved one to their follow-up appointments with Anca Breahna and the nursing staff. Help communicate any concerns or questions they may have, and take notes on any important instructions or recommendations provided by the medical team.
- Provide emotional support: Recovering from plastic surgery can be an emotional experience, and your loved one may face moments of frustration, anxiety, or self-doubt. Be patient, understanding, and supportive throughout the process. Encourage them to express their feelings openly and reassure them that healing takes time and that you’re there to support them every step of the way.
FAQs about Recovery after Plastic Surgery
How long should I plan to take off work to support my loved one’s recovery?
The amount of time you may need to take off work depends on the type of procedure your loved one underwent and the extent of their post-operative needs.
In general, it’s a good idea to plan for at least 3-5 days of dedicated support, especially during the initial phase of recovery.
If your loved one had a more extensive procedure or has additional needs, you may want to consider taking off more time or arranging for alternative support to ensure they receive the care and assistance they require.
Can I help my loved one shower or bathe after their surgery?
In most cases, patients will need to wait at least 24-48 hours before showering or bathing after surgery.
When your loved one is ready to clean themselves, you may need to assist them in getting in and out of the shower or bath safely.
Ensure they follow their surgeon’s specific instructions regarding wound care, dressing changes, and any water restrictions.
Help them gently pat the surgical site(s) dry and reapply any necessary dressings or compression garments.
What should I do if my loved one experiences nausea or vomiting after surgery?
Nausea and vomiting can be common side effects of anaesthesia and pain medication.
If your loved one experiences these symptoms, encourage them to take slow, deep breaths and sip on clear liquids such as water, tea, or ginger ale.
If nausea persists or vomiting occurs repeatedly, contact Anca Breahna’s team for guidance, as they may need to adjust the pain medication or recommend additional anti-nausea treatments.
How can I tell if my loved one is experiencing complications after surgery?
While some discomfort, swelling, and bruising are normal after plastic surgery, certain signs may indicate complications. These include:
- Excessive pain or pain that worsens over time
- Significant swelling or bruising that seems to be rapidly increasing
- Redness, warmth, or tenderness around the surgical site(s) that may suggest an infection
- Discharge or drainage from the incision sites that is excessive, foul-smelling, or contains pus
- Fever, chills, or severe headaches
How can I support my loved one’s emotional well-being during recovery?
Recovering from plastic surgery can be an emotional rollercoaster. To support your loved one’s emotional well-being:
- Encourage open communication and listen to their concerns and feelings without judgment
- Offer reassurance and remind them that healing takes time and patience
- Help them focus on positive progress and celebrate small milestones along the way
- Encourage them to engage in relaxing and enjoyable activities that don’t require physical exertion
- If they experience persistent feelings of sadness, anxiety, or despair, encourage them to reach out to a mental health professional for additional support
Remember, your role as a support person is invaluable, and your presence, understanding, and assistance can make a significant difference in your loved one’s recovery journey.
Further Reading about Plastic Surgery
- Read more about Preparing for Surgery
- Read more about Risks and Complications of Surgery
- Read more about Recovery after Plastic Surgery
- Read more about How to Lose Weight before Surgery
- Read more about Smoking and Vaping before/ after Surgery
 Ms Anca Breahna, PhD, MSc, FEBOPRAS, FRCS (Plast) is a highly regarded Consultant Plastic Surgeon specialising in the field of Aesthetic and Reconstructive Plastic Surgery. Anca performs a range of
Ms Anca Breahna, PhD, MSc, FEBOPRAS, FRCS (Plast) is a highly regarded Consultant Plastic Surgeon specialising in the field of Aesthetic and Reconstructive Plastic Surgery. Anca performs a range of 